“Public Health and Hospitals” being a State subject, the primary responsibility of strengthening public healthcare system, including for provision of quality healthcare and advanced treatment and diagnostic facilities, lies with the respective State Governments. However, under National Health Mission (NHM), technical and financial support is provided to the States/UTs to strengthen the public healthcare delivery at public healthcare facilities.
To address the healthcare challenges, particularly in rural areas, the National Rural Health Mission (NRHM) was launched in 2005 to supplement the efforts of the State/UT governments to provide accessible, affordable and quality healthcare to all those who access public health facilities. Currently, NRHM is a sub-mission of National Health Mission (NHM). NUHM was also launched in 2013 as a sub-mission of NHM.
NHM support is provided to States/ UTs for setting up of new facilities as per norms and upgradation of existing facilities for bridging the infrastructure gaps based on the requirement posed by them.
NHM support is also provided for provision of a range of free services related to maternal health, child health, adolescent health, family planning, universal immunisation programme, and for major diseases such as Tuberculosis, vector borne diseases like Malaria, Dengue and Kala Azar, Leprosy etc.
Other major initiatives supported under NHM include Janani Shishu Suraksha Karyakram (JSSK) (under which free drugs, free diagnostics, free blood and diet, free transport from home to institution, between facilities in case of a referral and drop back home is provided), Rashtriya Bal Swasthya Karyakram (RBSK) (which provides newborn and child health screening and early interventions services free of cost for birth defects, diseases, deficiencies and developmental delays to improve the quality of survival), implementation of Free Drugs and Free Diagnostics Service Initiatives, PM National Dialysis Programme and implementation of National Quality Assurance Framework in all public health facilities including in rural areas.
Mobile Medical Units (MMUs) & Tele-consultation services are also being implemented to improve access to healthcare particularly in rural areas.
As part of Ayushman Bharat, the States are supported for establishment of 1.5 lakh Health and Wellness Centres across the country by December, 2022 for provision of comprehensive primary care that includes preventive healthcare and health promotion at the community level with continuum of care approach. Further Ayushman Bharat, Pradhan Mantri Jan Arogya Yojana (AB-PMJAY) provides health coverage up to Rs 5 Lakh per family per year to around 1074 crore poor and vulnerable families as per Socio Economic Caste Census (SECC).
In the 15 years of implementation, the NHM has enabled achievement of the Millennium Development Goals (MDGs) for health. It has also led to significant improvements in maternal, new-born, and child health indicators, particularly for maternal mortality ratio, infant and under five mortality rates, wherein the rates of decline in India are much higher than the global averages and these declines have accelerated during the period of implementation of NHM. The major achievements under NHM are given at Annexure.
Achievements of NHM
Improvements in Core Health Outcomes:
Reduction in OOPE: The average medical expenditure per hospitalization and childbirth also declined in this period, from Rs. 5636 to Rs. 4290 in rural areas, and Rs. 7670 to Rs. 4837 in urban areas for hospitalization and from Rs. 1587 to Rs. 1324 in rural areas and Rs. 2117 to Rs. 1919 in urban areas for institutional delivery, indicating the impact of NHM in reduction of Out of Pocket Expenditures for health care.
Maternal Mortality Rate (MMR) has declined from 556/lakh live births in 1990 to 113/lakh live births in 2016-2017. Rate of decline of MMR in India at 77% is much higher than global average decline of 44% over the same period.
Infant Mortality Rate (IMR), declined from 80 in 1990 to 32 in the year 20181.
Under 5 Mortality Rate (U5MR), declined from 52 in 2012 to 36 in 2018,
Total Fertility Rate (TFR) declined from 2.3 in 2013 to 2.2 in the year 20181.
The incidence of Tuberculosis per 1,00,000 population reduced from 234 in 2012 to 193 in 2019. The mortality due to TB per 1,00,000 population also reduced from 42 in 2012 to 33 in 2019.
The number of districts that achieved the target of leprosy elimination increased from 543 districts in 2011-2012 to 554 by March 2017 and to 571 districts by March 2018. The prevalence rate of Leprosy reduced to less than 1/10000 population in 610 Districts in 2020.
For Malaria, Annual Parasitic Index (API) was sustained at levels of less than 1 and declined from 0.89 in 2014 to 0.32 in 2018, and 0.25, in 2019. Malaria cases and deaths declined from 21.27% and 20% respectively in 2019 from 2018.
By the end of December 2019, 94% Kala-azar endemic blocks have achieved the elimination target of <1 KA case per 10,000 population at block level.
The National target for sustaining Dengue related case fatality rate to less than 1% was met. Dengue related case fatality rate in 2014 was 0.3% and reduced to 0.1% in 2019.
The prevalence of blindness (visual acuity <3/60) has reduced to 0.36% in 2019) from 0.68% in 2010.
There is a 17.3% relative reduction in prevalence of tobacco use from 34.6% to 28.6% from 2009-10 to 2016-17.
Increased Access to Health Services:
As a result of the health systems strengthening efforts of NHM, the proportion of those seeking care from public health facilities, increased from 28.3% to 32.5% in rural areas and 21.2% to 26.2% in urban areas between 2014 to 2017.; and utilization of public health facilities for institutional deliveries increased from 56% to 69.2% in rural areas and from 42% to 48.3% in urban areas.
Growth in Public Health Facilities:
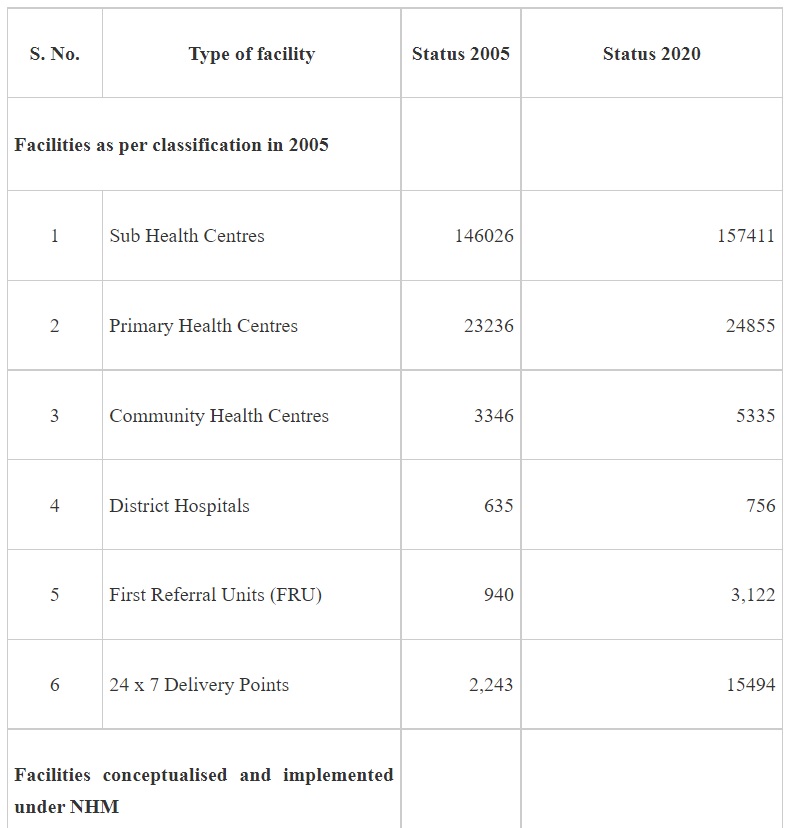
NHM adopts a health system approach and targets to build a network for public health facilities with Health & Wellness Centres at the grassroot level and District Hospitals, with robust referral linkage, to offer Comprehensive primary and secondary care services to citizens. The growth in the number of facilities at various levels since 2025 is given in Table 1 -
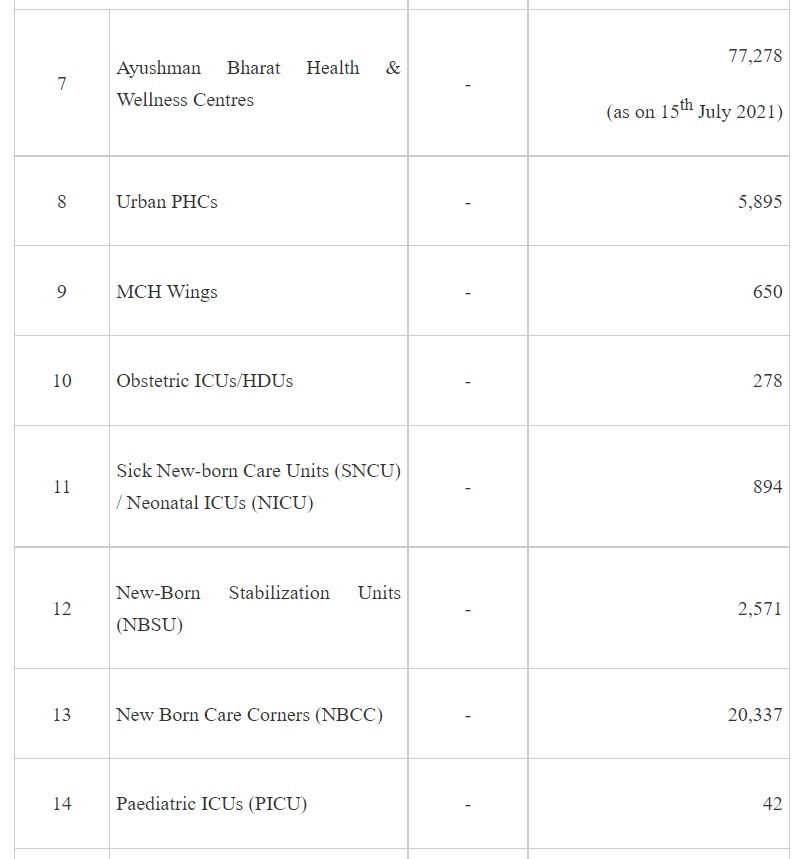

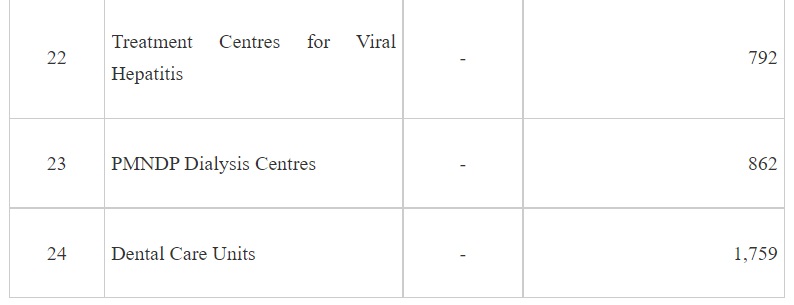
It may be seen from the above that implementation of NHM has not only contributed to increase in the institutional capacities for service delivery but also has led to development of capacities for targeted interventions of the various National Programmes under the NHM.
3. Equitable development: There was also a sustained focus on the health of tribal populations, those in Left Wing Extremism areas, and the urban poor. A more recent effort at ensuring equity in access and use, is the Aspirational district initiative, in which 115 districts across 28 states, with weak social and human development indicators have been identified for allocation of additional resources and capacity enhancement to catch up with more progressive districts.
4. National Ambulance Services: At the time of launch of NRHM (2005), ambulance networks were non-existent. So far, 20,990 Emergency Response Service Vehicles are operational under NRHM. Besides 5,499 patient transport vehicles are also deployed, particularly for providing “free pickup and drop back” facilities to pregnant women and sick infants.
5. Human Resource Augmentation: NHM supports states for engaging of service delivery HR such as doctors, nurses and health workers and also implements the world’s largest community health volunteer programme through the ASHAs. More than 10 lakhs ASHAs and ASHA facilitators are engaged under NHM. NHM has also supported states to acquire staff with skills in public health, finance, planning, management and M&E to plan and implement interventions, freeing up clinical staff to deliver health services. Differential remuneration and incentives linked to remote/underserved areas of posting, resulted in increased availability and retention of HR in difficult and remote areas. Human Resource Information System (HRIS) is a key administrative HR reform implemented under NHM for regular and contractual staff, providing comprehensive real time information on the HR posted in facilities and in managerial positions, facilitating salary payments and transfer postings. NHM invests in capacity building and mentoring for all cadres of personnel, with a focus on multi-skilling and task sharing to address HR shortages.
6. Health Sector Reforms: The National Health Mission (NHM) enabled the design and implementation of reforms specifically related to Governance (Decentralized Management Units, and creation of flexibility in administrative and fund management decisions, creation of Rogi Kalyan Samitis, establishment of community collectives for accountability, such as the Village Health, Sanitation and Nutrition Committees and Mahila Arogya Samitis), Procurement (creating the institutional mechanisms needed for effective procurement modalities such as the Medical services Corporations in several states, improve supply chain and logistics management, and expand procurement capacity), and Technology (to facilitate reporting, follow up of mothers and children in need of services, IEC and for tracking vaccine use).
7. Addressing high Out-of-Pocket Expenditure (OOPE): Recognising the need for reducing the current high levels OOPE, and that, almost 70% of the OOPE is on account of drugs and diagnostics, the Free Drugs and Free Diagnostics Services Initiatives have been implemented under the NHM. The Essential Drugs Lists (EDL) and the Essential Diagnostics Lists have been notified and are periodically updated to include more essential drugs based on new initiatives undertaken. These interventions coupled with strengthening of health facilities’ capacities to deliver an expanded range of services, closer to communities, teleconsultation services are leading to significant reduction in OOPE.
NHM supported health system reforms have resulted in development of resilient health systems, albeit at different stages of maturity that enable successful scaling up of existing interventions and the addition of newer reforms given the rapid transitions from rural to urban, gradual demographic transition to aging populations, increasing burden of chronic diseases, and the emergence of newer infectious diseases.
Of note is that the NHM reforms were oriented towards addressing inequity, across and within states. A study done in 2020 by the National Institute of Public Finance and Policy (NIPFP) on health spending in states under NHM, suggests that NHM contributed to reduction of inequality in health spending across states and added funds to the lower tiers of the health pyramid.
The Union Minister of State for Health and Family Welfare, Dr. Bharati Pravin Pawar stated this in a written reply in the Rajya Sabha here today.