
Situation at a glance
Since the last Disease Outbreak News on this event was published on 23 August 2024, three additional countries and one territory (Ecuador, Guyana, Panama and Cayman Island) have reported confirmed Oropouche virus disease in the Region of the Americas in 2024. In addition, imported Oropouche cases have been reported from Canada, the United States of America and countries of the European Region. As of 25 November 2024, a total of 11 634 confirmed Oropouche cases, including two deaths, have been reported in the Region of the Americas, across ten countries and one territory: Bolivia (Plurinational State of), Brazil, Canada, Cayman Islands, Colombia, Cuba, Ecuador, Guyana, Panama, Peru and the United States of America. Based on available information, WHO assesses the overall public health risk posed by this virus to be high at the regional level and low at the global level. As the arbovirus season is starting in the region, WHO urges countries at risk to strengthen epidemiological and entomological surveillance and to reinforce preventive measures in the population. This is crucial due to the geographical expansion of the virus and the possible new vectors and transmission routes, including vertical transmission, that could affect both the general population and vulnerable groups, such as pregnant women, their fetuses, and newborns.
Description of the situation
Since the last Disease Outbreak News on this event was published on 23 August 2024, three additional countries and one territory (Ecuador, Guyana, and Panama) have reported confirmed Oropouche virus disease in the Region of the Americas. In addition, imported Oropouche cases were reported from the Cayman Islands, Canada, the United States of America and a few countries in the European Region.
Between 1 January and 25 November 2024, 11 634 confirmed Oropouche cases, including two deaths, have been reported in the Region of the Americas: Bolivia (Plurinational State of) (356 cases), Brazil (9563 cases, including two deaths), Canada (two imported cases), Cayman Island (one imported case), Colombia (74 cases), Cuba (603 cases), Ecuador (two cases), Guyana (two cases), Panama (one case), Peru (936 cases), and the United States of America (94 imported cases). Additionally, imported Oropouche cases have been reported in countries in the European Region (30 cases) (1).
Cases and consequences of vertical transmission of Oropouche virus infection have been reported in Brazil and Cuba. Brazil has confirmed three cases of vertical transmission (two cases of fetal death and one case of congenital anomaly) and reported that under investigation are 15 fetal deaths, five spontaneous miscarriages, and three cases of congenital anomalies.[1] Additionally, in September, Cuba confirmed a case of congenital anomaly with two further cases under investigation.
Figure 1. Number of confirmed Oropouche cases in 2024 by country and epidemiological week of symptom onset Region of the Americas*
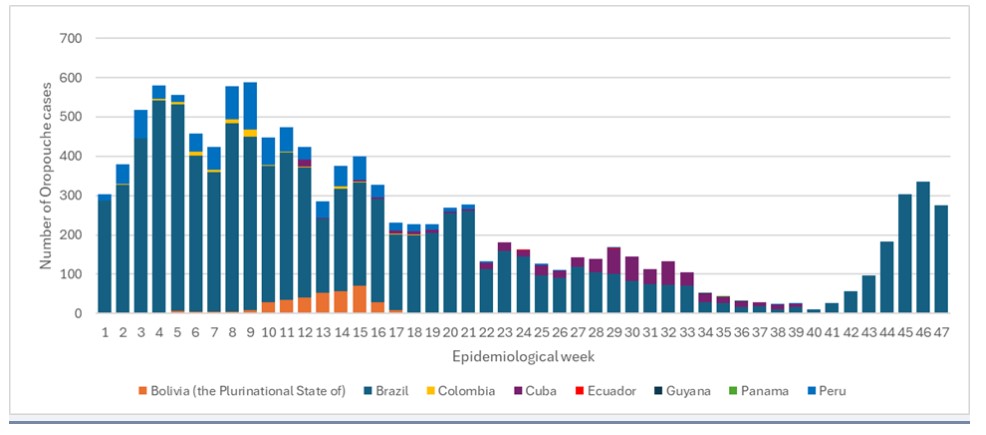
*Source: Adapted and reproduced by PAHO/WHO from the data reported by the respective countries.
The following is a summary of the situation in the countries that have reported confirmed Oropouche cases in the Americas as of 25 November 2024.
The Plurinational State of Bolivia: Between 1 January and 5 October 2024, there were 356 Oropouche cases confirmed by reverse transcription polymerase chain reaction (RT-PCR) testing. Transmission has been reported in three departments: La Paz with 75.3% of cases (268 cases), followed by Beni with 21.3% of cases (76 cases), and Pando with 3.4% of cases (12 cases). Cases have been reported in 16 municipalities that are considered endemic for this disease, with the highest proportion of cases reported in the municipalities of Irupana, La Paz, with 33% of cases; followed by La Asunta, La Paz, with 13% of cases; Chulumani, La Paz, and Guayaramerín, Beni, with 12% each.
Half of the cases are female (179 cases) and the age group with the highest number of cases is the 30-39 years age group accounting for 20% of cases (70 cases). No deaths have been recorded that could be associated with OROV infection. In addition, between 23 March and 13 April 2024, ten cases of coinfection of Oropouche and dengue were reported in patients in three municipalities of the department of La Paz, all of whom tested positive for dengue by RT-PCR with DENV-1 (two cases) and DENV-2 (eight cases) serotyping (2).
Brazil: Between 1 January and 25 November 2024, 9563 Oropouche cases were confirmed by RT-PCR. Most cases have been reported in municipalities in the northern states; however, to date, cases have been reported in 22 of the country's 27 states. The Amazon region, an area considered endemic for Oropouche, accounts for 70% of the cases reported in the country, with seven states reporting cases: Amazonas (3231 cases), Rondônia (1711 cases), Acre (273 cases), Roraima (277 cases), Pará (157 cases), Amapá (128 cases), and Tocantins (eight cases) (3). Additionally, autochthonous transmission has been documented in 15 non-Amazonian states, some of which had not previously reported cases: Bahia (889 cases), Espírito Santo (1763 cases), Ceará (249 cases), Minas Gerais (194 cases), Santa Catarina (178 cases), Pernambuco (144 cases), Rio de Janeiro (116 cases), Alagoas (116 cases), Sergipe (34 cases), Maranhão (33 cases), Piauí (30 cases), Mato Grosso (18 cases), São Paulo (eight cases), Paraíba (five cases) and Mato Grosso do Sul (one case)(3, 4).
Over half of the cases (52%; 4995) are male and the age group with the highest number of cases is 20-29 years, with 21% of cases (1963 cases) (3).
Brazil’s IHR National Focal Point (NFP) reported two fatal cases of OROV infection detected retrospectively in the state of Bahia1 and six cases are under investigation: one in the state of Parana, with probable source of infection in the state of Santa Catarina, two in Espírito Santo, one in Acre, one in Alagoas, and one in Mato Grosso (4).[2] Additionally, on 12 August 2024, Brazil reported a case of encephalitis associated with OROV. The case is a male resident of the state of Piauí (3).[3] As of 16 November 2024, three cases of vertical transmission have been confirmed:[4] two cases of fetal death: one in Pernambuco and one in Ceará; and one case of congenital anomaly in Acre. As for cases under investigation in the country, 15 cases of fetal death in Pernambuco (15 cases), three cases of congenital anomaly in Acre (two cases) and Bahia (one case), and five spontaneous miscarriages in Pernambuco have been identified (3-5).
Colombia: Between 1 January and 5 October 2024, 74 confirmed Oropouche cases have been reported in three departments of the country: Amazonas (70 cases), Caqueta (one case), and Meta (one case); additionally, two cases were identified in travellers from Tabatinga, Brazil. The cases were identified through a retrospective laboratory case-finding strategy implemented in 2024 by the National Institute of Health of Colombia based on dengue surveillance (38 cases) and through investigation of febrile syndrome cases (36 cases). Over half of the cases (51.4%; 38) were female and the age group with the highest number of cases was 10-19 years, with 36.5% of the cases (27 cases). No deaths have been recorded that could be associated with OROV infection.
Six cases of coinfection with dengue were reported in the department of Amazonas, four in the municipality of Leticia (two with DENV-1 and two with DENV-2), and one in the municipality of Puerto Nariño (DENV-3), and in the department of Meta, one in the municipality of Guamal (DENV-4). Regarding the surveillance of cases of vertical transmission and its consequences, up to 3 October 2024, two cases of Oropouche have been identified in pregnant women, both from Leticia, aged 18 years (onset of symptoms at 29 weeks of gestation) and 22 years (onset of symptoms at 34 weeks of gestation), respectively. Both evolved favorably and their children were born without complications. To date, none of the infants show evidence of congenital anomalies, neurological syndromes or neurodevelopmental disorders.[5]
Cuba: Between 27 May and 25 November 2024, a total of 603 confirmed cases were reported. Cases continue to be identified through surveillance for non-specific febrile syndrome, with cases recorded in 109 municipalities in the 15 provinces of the country. The provinces of Havana (174 cases), Santiago de Cuba (75 cases), Pinar del Rio (47 cases), and Cienfuegos (39 cases) accounted for 55% of confirmed cases.[6]
More than half of the cases were female (55%, 331) and the highest proportion of cases was recorded in the 19-54 age group (53%, 320). On 19 September 2024, Cuba reported three cases of Guillain-Barré syndrome (GBS) associated with OROV. The three cases, two females and one male aged 51, 53, and 64 years respectively, presented with onset of symptoms in June. The cases are residents of the province of Santiago de Cuba, in the municipalities of San Luis (one case) and Santiago de Cuba (two cases). Serum, cerebrospinal fluid (CSF) and urine samples were collected and tested positive with RT-PCR for OROV.
Seven cases of Oropouche were identified in pregnant women, two of whom delivered live babies without any congenital anomalies being detected. On the other hand, three cases of congenital anomalies of the central nervous system with suspected infectious aetiology have been identified through the national antenatal referral service, of which one has undergone virological testing with a positive result for OROV in fetal heart blood; the other two cases are under investigation.
Ecuador: As of 5 October 2024, two laboratory-confirmed cases of Oropouche virus disease were reported, which were detected during a retrospective analysis of dengue-negative samples by the National Institute of Public Health Research (INSPI per its acronym in Spanish). The first case occurred in a 62-year-old from Bolivar province who developed symptoms on 11 June. The second case occurred in a 36-year-old from Los Rios province who developed symptoms on 17 July. Both patients have no history of recent travel. None of the cases required hospitalization and have fully recovered.
Guyana: Between 8-14 September 2024, two laboratory-confirmed cases of Oropouche virus disease were reported, being the first detection of this disease in the country. The first case was a 47-year-old who presented with symptoms on 21 August 2024. The case sought medical attention on 24 August 2024. Blood samples were collected, and RT-PCR test performed on 3 September was positive for OROV. The second case reported from a 42-year-old who presented with symptoms on 2 September 2024. The case sought medical attention on 3 September 2024. Blood samples was collected, and RT-PCR tests performed on 7 September was positive for OROV. Both cases had resided in the same geographical area in the Mahaica-Berbice region, for at least 14 days prior to symptom onset and neither has reported history of travel.
Panama: On 15 November 2024, the Panama IHR National Focal Point reported the first confirmed case of Oropouche virus diseases in 2024. The case was confirmed by the Gorgas Commemorative Institute of Health studies (ICGES, per its acronym in Spanish) laboratory in Panama. The case age is between 30 and 35 years from Province of Coclé with a recent travel history within the country. The case reported onset symptoms on 27 August 2024, and was diagnosed with suspected dengue. The case didn’t require hospitalization and recovered at home. This case was detected through the laboratory surveillance strategy, which involved testing a sample from a patient with dengue-like symptoms who initially tested negative for DENV. On 15 November, the case was confirmed for OROV by RT-PCR. Although recovered, the case is currently under investigation, as the exact site of exposure and transmission has not yet been determined.
Peru: Between 1 January and 5 October 2024, 936 confirmed Oropouche cases have been reported in eight departments of the country. The departments are Loreto (466 cases), Madre de Dios (312 cases), Ucayali (138 cases), Huanuco (15 cases), Junin (two cases), Tumbes (one case), San Martin (one case), and Puno (one case). Over half of the cases (51%; 476) were male, and the age group with the highest number of cases was 30-39 years, with 37% of the cases (348 cases). There were no deaths and no reports of possible vertical transmission reported from the country.
Imported cases in non-endemic countries and territories
Canada: As of 21 September 2024, Canada confirmed two Oropouche cases with a history of travel to Cuba.
Cayman Islands: On 16 September 2024, the Caribbean Public Health Agency (CARPHA) confirmed an imported case of Oropouche virus in an adult woman from the Cayman Islands who had travelled to Cuba. The patient developed symptoms, including fever and muscle pain, on 10 August after returning. The initial test for Oropouche virus in the Cayman Islands on 12 August was positive and confirmed at the CARPHA reference laboratory from a convalescent sample collected on 15 August.
United States of America: As of 8 October 2024, 94 imported cases of Oropouche virus disease were identified in the states of Florida (90 cases), California (one case), Colorado (one case), Kentucky (one case), and New York (one case). The median age of the cases was 51 years (ranging from 6 to 94 years) and 48% were female. A total of three cases were hospitalized. Two of the cases presented with neuroinvasive disease, no deaths were reported, and all cases had a history of travel to Cuba.
Additionally, between 2 June and 20 July 2024, 30 imported cases of Oropouche have been identified in three countries of the WHO European Region: Germany (three cases), Spain (21 cases), and Italy (six cases); 20 of these cases had a history of travel to Cuba and one to Brazil, these cases are of the first cases registered in this region.
Epidemiology
Oropouche virus disease is an arboviral disease caused by the Oropouche virus (OROV), a segmented single-stranded RNA virus that is part of the genus Orthobunyavirus of the Peribunyaviridae family. The virus has been found to circulate in Central and South America and the Caribbean. OROV can be transmitted to humans primarily through the bite of the Culicoides paraensis midge, found in forested areas and around water bodies, or certain Culex quinquefasciatus mosquitoes. It is suspected that viral circulation includes both urban epidemic and sylvatic cycles. In the sylvatic cycle, primates, sloths, and perhaps birds are vertebrate hosts, but a definitive arthropod vector has not been identified. In the urban epidemic cycle, humans are the amplifying host and OROV is transmitted primarily through the bite of the Culicoides paraensis midge. Vertical transmission has been documented in Brazil and Cuba and some cases are being investigated further. To date, there is no evidence of other modes of human-to-human OROV transmission.
The disease symptoms are similar to dengue, starting four to eight days (between three to 12 days) after the infective bite. The onset is sudden, usually with fever, intense headache, joint stiffness, pain, chills, and sometimes persistent nausea and vomiting, for up to seven days. Up to 60% of cases have a relapse of symptoms after the fever stops. Most cases recover within seven days, however, in some patients, convalescence can take weeks. Severe clinical presentation is rare, but it may result in aseptic meningitis during the second week of the disease.
There is no specific antiviral treatment or vaccine for Oropouche virus disease. A recent publication describes the presence of Oropouche replication-competent virus in bodily fluids such as blood, serum, urine and even semen, found in samples of a patient diagnosed with the disease upon returning to Italy after a trip to Cuba. The virus was detected in cultures up to 16 days after symptoms onset. However, the results are not conclusive to confirm sexual transmission of the disease and there have been no reports of this kind of transmission.
Public health response
Regional level:
Epidemiological alerts and updates have been issued to alert Member States and recommend actions to be implemented. Information has also been disseminated through regional and national webinars for health personnel.
Algorithms for laboratory testing have been developed and disseminated. Training on molecular testing (RT-PCR) and characterization (whole genome sequencing) has been provided through workshops or remote assistance, and critical reagents have been distributed. As a result of regional and national efforts, molecular testing capacity is available in 23 of the 33 countries in Latin America and the Caribbean. WHO is working to expand these capacities as necessary.
The available clinical information has been reviewed to recommend interim case definitions (suspected, probable, and confirmed, vertical transmission).
A virtual collaboration space has been created at the regional level to develop epidemiological analytics of the disease.
Generic research protocols for the characterization of pregnancy outcomes in infants from OROV-exposed pregnant individuals have been drafted and shared.
WHO experts are providing support in countries that are experiencing outbreaks.
Development and publication of Interim guidance on entomological surveillance and prevention measures for Oropouche virus vectors.
Regional workshop on the biology, ecology and surveillance of insects of the genus Culicoides (Diptera: Ceratopogonidae) vectors of the Oropouche virus (OROV) in the Americas was held in FIOCRUZ Manaus-Brazil from 18 to 22 November 2024, with the participation of eight countries.
WHO risk assessment
In the Region of the Americas, outbreaks of Oropouche virus disease have occurred historically in the Amazon region. Numerous outbreaks of OROV disease have been reported in both rural and urban communities in Brazil, Colombia, Ecuador, French Guiana, Panama, Peru, and Trinidad and Tobago.
The ongoing outbreak highlights the need to strengthen epidemiological and entomological surveillance and to reinforce preventive measures in the population. This is crucial due to the expansion of the virus's transmission area and the growing need to better understand the disease spectrum, including possible new transmission routes and new vectors that could affect both the general population and vulnerable groups, such as pregnant women, their fetuses, and newborns.
Based on available information, WHO assesses the overall public health risk posed by this virus to be high at the regional level and low at the global level.
WHO advice
The proximity of midge vector breeding sites to human habitations is a significant risk factor for OROV infection. Prevention strategies are based on control measures against the arthropod vectors and on personal protection measures. Vector control measures rely on reducing midge populations through the control of breeding sites, achieved by reducing the number of natural and artificial water-filled habitats that support midge larvae, thereby reducing the adult midge populations around at-risk communities. Personal protection measures rely on the prevention of midge bites using mechanical barriers (mosquito nets), insect repellant devices, repellent-treated clothing and mosquito repellents. Chemical insecticides such as deltamethrin and N,N-Diethyl-meta-toluamide (DEET) have been demonstrated to be effective in providing protection against bites from Culicoides and Culex species.
Given its clinical presentation and considering that this is the beginning of the arbovirus season in the Southern cone part of the Region of the Americas, strengthen epidemiological (including maternal health and birth defects data) and entomological surveillance, laboratory diagnosis is essential to confirm cases, characterize the outbreak, and monitor disease trends.
Since it is an emerging and poorly identified arbovirus in the Americas, the detection of a positive sample and confirmation of a case requires the use of Annex 2 of the IHR and its consequent notification through the established channels of the IHR.
WHO advises against applying any travel or trade restrictions based on the current information available on this event.
About WHO
The World Health Organization provides global leadership in public health within the United Nations system. Founded in 1948, WHO works with 194 Member States, across six regions and from more than 150 offices, to promote health, keep the world safe and serve the vulnerable. Our goal for 2019-2023 is to ensure that a billion more people have universal health coverage, to protect a billion more people from health emergencies, and provide a further billion people with better health and wellbeing.