
Late-breaking Phase III results show subcutaneous injection was non-inferior to intravenous infusion based on OCREVUS levels in the blood over 12 weeks
OCREVUS subcutaneous injection was comparable to IV infusion in providing rapid and sustained depletion of B cells and near-complete suppression of MRI lesion activity in the brain over 24 weeks
The safety profile of OCREVUS subcutaneous injection was consistent with the well-established safety profile of OCREVUS IV infusion
The 10-minute subcutaneous injection has potential to improve the treatment experience and expand usage for people with multiple sclerosis (MS) in centres with IV capacity limitations
Roche (SIX: RO, ROG; OTCQX: RHHBY) today announced late-breaking data from the Phase III OCARINA II study. Study results demonstrate the effect of OCREVUS® (ocrelizumab) as an investigational twice-yearly, 10-minute subcutaneous injection on pharmacokinetic, biomarker, and MRI measures in patients with relapsing or primary progressive multiple sclerosis (RMS or PPMS). The data will be presented in a poster at the 9th Joint ECTRIMS-ACTRIMS Meeting (European and Americas Committees for Treatment and Research in Multiple Sclerosis).
“We are pleased to share that OCREVUS 10-minute subcutaneous injection suppressed brain lesions as effectively as the intravenous infusion,” said Levi Garraway, M.D., Ph.D., Roche’s Chief Medical Officer and Head of Global Product Development. “Having this additional treatment option may improve the treatment experience for both patients and physicians, and we hope the twice-a-year dosing will offer the same high adherence and persistence.’’
OCREVUS subcutaneous injection was non-inferior to OCREVUS IV infusion as measured by OCREVUS levels in the blood of patients (area under the serum concentration time curve) from day 1 to 12 weeks (3500 day*µg/mL for subcutaneous injection vs. 2750 day*µg/mL for IV infusion). Peak OCREVUS blood (serum) concentrations were similar for subcutaneous injection (132 µg/mL) and IV infusion (137 µg/mL).
OCREVUS subcutaneous injection provided rapid, sustained and near-complete B-cell depletion that was similar to OCREVUS IV infusion (97% and 98% of patients respectively had B cells levels of 5 cells/µL or less when first measured at 14 days), which was sustained over 24 weeks. At the time of analysis, approximately half the patients in the study had reached 24 weeks of treatment.
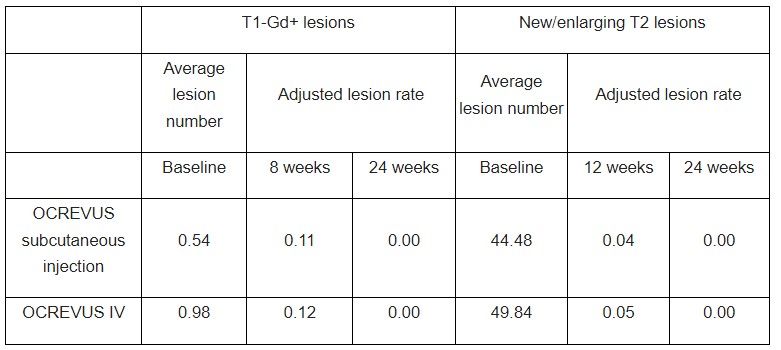
Both OCREVUS subcutaneous injection and OCREVUS IV infusion resulted in rapid and near-complete suppression of MRI lesion activity by 24 weeks, with most patients having no T1 gadolinium-enhancing (T1-Gd+) lesions, which are markers of active inflammation, and no new/enlarging T2 lesions, which represent the amount of disease burden or lesion load at 24 weeks.
The safety profile of OCREVUS subcutaneous injection was consistent with the well-established safety profile of OCREVUS IV infusion. No new safety signals were identified for OCREVUS subcutaneous injection. The most common adverse events in the OCREVUS subcutaneous injection group were injection reactions (48% of all exposed patients), all of which were either mild or moderate. The most common AEs in the OCREVUS IV infusion group were infusion-related reactions (17%). A total of 4 and 7 serious AEs were experienced by 3 (2.5%) and 4 (3.4%) patients in the OCREVUS subcutaneous and IV infusion groups, respectively.
The OCREVUS twice-yearly, 10-minute subcutaneous injection is healthcare provider administered and designed to be delivered without the need for IV infrastructure, so it has the potential to expand the usage of OCREVUS in treatment centres without IV infrastructure or those with IV capacity limitations. This provides an additional delivery option so that OCREVUS can be matched to the individual needs of people with MS and healthcare professionals.
The OCARINA II data will be submitted to health authorities around the world in the coming months. Roche is committed to advancing innovative clinical research programmes to broaden the scientific understanding of MS, further reduce disability progression in RMS and PPMS and improve the treatment experiences for those living with the disease.
About the subcutaneous formulation of OCREVUS (ocrelizumab)
The investigational subcutaneous formulation combines OCREVUS with Halozyme Therapeutics’ Enhanze® drug delivery technology.
OCREVUS is a humanised monoclonal antibody designed to target CD20-positive B cells, a specific type of immune cell thought to be a key contributor to myelin (nerve cell insulation and support) and axonal (nerve cell) damage. This nerve cell damage can lead to disability in people with MS. Based on preclinical studies, OCREVUS binds to CD20 cell surface proteins expressed on certain B cells, but not on stem cells or plasma cells, suggesting that important functions of the immune system may be preserved.
The Enhanze drug delivery technology is based on a proprietary recombinant human hyaluronidase PH20 (rHuPH20), an enzyme that locally and temporarily degrades hyaluronan – a glycosaminoglycan or chain of natural sugars in the body – in the subcutaneous space. This increases the permeability of the tissue under the skin, allowing space for large molecules like OCREVUS to enter, and enables the subcutaneous formulation to be rapidly dispersed and absorbed into the bloodstream.
OCREVUS IV is the first and only therapy approved for both RMS (including relapsing-remitting MS [RRMS] and active, or relapsing secondary progressive MS [SPMS], in addition to clinically isolated syndrome [CIS] in the U.S.) and PPMS. OCREVUS IV is administered by intravenous infusion every six months. The initial dose is given as two 300 mg infusions given two weeks apart. Subsequent doses are given as single 600 mg infusions.
About the OCARINA II study
OCARINA II is a Phase III, global, multicentre, randomised study evaluating the pharmacokinetics, safety and radiological and clinical effects of the subcutaneous formulation of OCREVUS compared with OCREVUS intravenous (IV) infusion in 236 patients with relapsing MS (RMS) or primary progressive MS (PPMS). The primary endpoint is non-inferiority in area under the serum concentration time curve (AUC) from day 1 to 12 weeks after subcutaneous injection compared to IV infusion. Secondary endpoints include maximum serum concentration (Cmax) of OCREVUS, the total number of active, gadolinium-enhancing T1 lesions at 8 and 12 weeks, and new or enlarging T2 lesions at 12 and 24 weeks, as well as safety and immunogenicity outcomes. Exploratory endpoints include patient-reported outcomes.
About multiple sclerosis
Multiple sclerosis (MS) is a chronic disease that affects more than 2.8 million people worldwide. MS occurs when the immune system abnormally attacks the insulation and support around nerve cells (myelin sheath) in the central nervous system (brain, spinal cord and optic nerves), causing inflammation and consequent damage. This damage can cause a wide range of symptoms, including muscle weakness, fatigue and difficulty seeing, and may eventually lead to disability. Most people with MS experience their first symptom between 20 and 40 years of age, making the disease the leading cause of non-traumatic disability in younger adults.
People with all forms of MS experience disease progression – permanent loss of nerve cells in the central nervous system – from the beginning of their disease even if their clinical symptoms aren’t apparent or don’t appear to be getting worse. Delays in diagnosis and treatment can negatively impact people with MS, in terms of their physical and mental health, and contribute to the negative financial impact on the individual and society. An important goal of treating MS is to slow, stop and ideally prevent disease activity and progression as early as possible.
Relapsing-remitting MS (RRMS) is the most common form of the disease and is characterised by episodes of new or worsening signs or symptoms (relapses) followed by periods of recovery. Approximately 85% of people with MS are initially diagnosed with RRMS. The majority of people who are diagnosed with RRMS will eventually transition to secondary progressive MS (SPMS), in which they experience steadily worsening disability over time. Relapsing forms of MS (RMS) include people with RRMS and people with SPMS who continue to experience relapses. Primary progressive MS (PPMS) is a debilitating form of the disease marked by steadily worsening symptoms but typically without distinct relapses or periods of remission. Approximately 15% of people with MS are diagnosed with the primary progressive form of the disease. Until the FDA approval of OCREVUS, there had been no FDA-approved treatments for PPMS.
About Roche in Neuroscience
Neuroscience is a major focus of research and development at Roche. Our goal is to pursue ground-breaking science to develop new treatments that help improve the lives of people with chronic and potentially devastating diseases. Roche and Genentech are investigating more than a dozen medicines for neurological disorders, including MS, spinal muscular atrophy, neuromyelitis optica spectrum disorder, Alzheimer’s disease, Huntington’s disease, Parkinson’s disease, acute ischemic stroke, Duchenne muscular dystrophy and Angelman syndrome. Together with our partners, we are committed to pushing the boundaries of scientific understanding to solve some of the most difficult challenges in neuroscience today.
About Roche
Roche is a global pioneer in pharmaceuticals and diagnostics focused on advancing science to improve people’s lives. The combined strengths of pharmaceuticals and diagnostics under one roof have made Roche the leader in personalised healthcare – a strategy that aims to fit the right treatment to each patient in the best way possible.
Roche is the world’s largest biotech company, with truly differentiated medicines in oncology, immunology, infectious diseases, ophthalmology and diseases of the central nervous system. Roche is also the world leader in in vitro diagnostics and tissue-based cancer diagnostics, and a frontrunner in diabetes management.
Founded in 1896, Roche continues to search for better ways to prevent, diagnose and treat diseases and make a sustainable contribution to society. The company also aims to improve patient access to medical innovations by working with all relevant stakeholders. More than thirty medicines developed by Roche are included in the World Health Organization Model Lists of Essential Medicines, among them life-saving antibiotics, antimalarials and cancer medicines. Moreover, for the twelfth consecutive year, Roche has been recognised as one of the most sustainable companies in the Pharmaceuticals Industry by the Dow Jones Sustainability Indices (DJSI).
The Roche Group, headquartered in Basel, Switzerland, is active in over 100 countries and in 2020 employed more than 100,000 people worldwide. In 2020, Roche invested CHF 12.2 billion in R&D and posted sales of CHF 58.3 billion. Genentech, in the United States, is a wholly owned member of the Roche Group. Roche is the majority shareholder in Chugai Pharmaceutical, Japan