Over the last few years, we have been repeatedly cautioned about India’s growing diabetes burden and its dubious distinction of being one of the ‘diabetes capitals of the world’. According to the International Diabetes Federation, there are 77 million Indians living with diabetes as of 2019, and that number is set to rise to 101 million by 2030 (International Diabetes Federation, 2019). The prevalence of diabetes in India has remained at 11.8% in the last four years, according to the National Diabetes and Diabetic Retinopathy Survey report released by the Ministry of Health and Family Welfare. These dire statistics should by now have driven us to take more concerted action against the disease. Now the message is loud and clear: diabetes is a grave public health threat to India and immediate action must be taken to bring it under control and reverse the rising trend.
There has been an unanimous opinion of the subject matter experts that diabetes must be managed at the multiple levels. First comes diagnosis. Many people live with slightly elevated blood sugar levels without realizing that they have entered what is known as the prediabetic stage. They need to be identified and cautioned on how to reverse this situation. So universal screening for diabetes becomes the first necessary step in bringing the rise of the disease under control. Related to this is the need for a continuous public education effort that reminds people about the lifestyle factors that contribute to the disease and how these should be handled. Finally, we need more support from our healthcare professionals in helping us tag the ‘undiagnosed’ amongst the population who could have been struggling with diabetes for some years without knowing it and inadvertently landed themselves into other health complications.
While the idea of having slightly high blood sugar levels can seem almost innocuous at first, over time it can cause damage to the larger and smaller blood vessels, nerves, and go on to affect the heart, kidneys, eyes and potentially every part of the body. This has a significant negative impact on the health of the patient, in addition to affecting productivity and putting a financial burden on the patient and/or family to manage the high out of pocket expenses. A significant challenge with diabetes is that it is usually a silent disease in the early stages. Which is why it is estimated that about half of all patients with diabetes are not even aware about their condition (International Diabetes Federation, 2019), even as it steadily damages the organs inside the body.
Forging partnerships that yield measurable results
The public private partnership (PPP) model has been in place for several years now and has found increasing acceptance in public health programs as well. That said, the success of such partnerships is contingent on the right players coming together to cohesively and collaboratively implement a diabetes control programmed in which the coalition partners have clear responsibilities in keeping with their inherent strengths and specialties and together formulate a scalable, replicable model for diabetes management that can be adopted across communities and states to tackle diabetes. Such a framework is an absolute necessity for us in India because it is virtually impossible for a single government or company or medical association or NGO to accomplish such a huge undertaking entirely on their own. Therefore, it is imperative to have strategically chosen partners working seamlessly together for a productive collaborative partnership to yield measurable results in the fight against diabetes in India.
The Screening-Awareness-Education Model
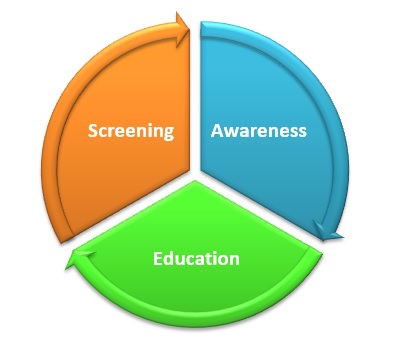
One such model that we believe can help us achieve measurable success in managing diabetes is the Screening-Awareness-Education model. The model rests on the three pillars of intervention that are crucial to reduce the number of those who transition from pre-diabetes to diabetes. d
Screening

India has a mere 30 to 35% screening rate for non communicable diseases (NCDs) such as diabetes(Joshi SR & Investigators., 2012), which is a dismal number and one that needs immediate intervention for improvement. While the primary health centres are doing an admirable job, they are usually overburdened in their daily efforts to cater to the immediate and urgent needs of patients in the community, which would give them little bandwidth to proactively take on a regular NCD screening programme.
However, community-based screening programmes are at the heart of a diabetes management intervention. Regular screening programmes can help diagnose the condition in patients who do not have any noticeable symptoms. Screening measures must also be linked to therapy interventions and lifestyle counseling. Patients who are diagnosed must be put on the right treatment, taught how to monitor their blood sugar regularly, and coached on healthy lifestyle habits such as regular physical activity and good diet. For a screening programme to be successful, it needs participation from multiple partners including government-run primary health centres and health officials, NGOs and private players who can together encourage people to come to the camp, counsel them on a healthy lifestyle, provide the necessary supply of blood sugar testing and monitoring kits, and ensure the centres are stocked with medication. The right public health partner can also help in a key outcome that is possible through screening programmes: data collection and analysis.
Data collected through screening programmes can be analysed by leading public health experts to yield information and insights on several key parameters such as
a. Prevalence of diabetes and pre-diabetes;
b. Average age at diagnosis;
c. Presence of complications at the time of diagnosis;
d. Understanding the behavior related to blood sugar monitoring;
e. Awareness of healthy lifestyle habits to help prevent diabetes or manage diabetes;
f. Barriers to accessing treatment; and Cost
These evidence-based insights can help to support and aid government policy development and determine what interventions need to be strengthened or what barriers need to be overcome for better diabetes management.
Awareness
Screening programs must run in tandem with public awareness initiatives on diabetes prevention and diabetes management. Several NGOs and service organizations have a widespread community reach across states and even the country. Bringing them aboard as partners in a diabetes programme can help to ensure that the messages reach the right target audience and the participation in screening programs increases. A critical component of successful awareness initiative is a sound communication outreach and the relevant material. It is essential to create easy-to-understand & implement literature on diabetes in multiple languages which can be distributed through the primary health centre, through healthcare workers or downloaded from a website. It is also important to harness all types of media channels and platforms including traditional print media, digital media and social media using platform-specific content that works for the audience to get the fundamental understanding on why people get diabetes, how to get diagnosed and how to manage treatment, living with diabetes and self-care to avoid the danger of tertiary complications.
We are only just beginning to understand that there are many health subjects which can easily be taught even to young children to start building their health knowledge base early in life. This is certainly true for diabetes.More and more we are seeing an increase in type 1 diabetes cases, also known as ‘juvenile diabetes’ because it emerges in childhood. So, school level exposure to information on T1D also serves to let all children learn more about adult diabetes. Children need to be made aware of the need to stay active and eat healthy, right from childhood rather than having to correct such habits later in life when it gets harder to do so. Of course, to work with children effectively, communication material needs to be age-specific, suitably simplified, creative, and communicated in a manner that helps the messages ‘stick’. Children can be great advocates for behaviour change at their homes, just if they are made to understand why a subject is important and relevant. Several NGOs that work with children or in schools can aid the execution of such a programme.
Education

While on-the-job training for healthcare workers is important, ongoing medical education needs a far more systematic and robust infrastructure and processes to be effective. For this reason, centres of excellence need to be set up to aid in training. These centres should be led by foremost diabetes experts and endocrinologists in the county and can provide the necessary research and training infrastructure on diabetes. The centres should also focus on the organization of virtual education workshops for healthcare professionals, online certification courses in association with the state government, and the development of in clinic educational materials. Their role can also be expanded to include webinars for patients, outreach modules for underprivileged children with diabetes through Integrated Personalised Diabetes Management.
The recent pandemic has demonstrated why it is imperative for health and pharma sector players to collaborate, to bring about big changes in the shortest possible time. There is much that can be learned from that and the response to contain many of the rapidly spreading diseases, such as diabetes, needs to have a similar sense of urgency. Diabetes is a health challenge that is fast becoming a health crisis. We are running out of time. But in this case, at least we know what we are up against, and we what we need to do. By bringing the right partners together, we can take quick and effective action so that instead of an ever-rising curve we start to see a steadily dipping trend in diabetes cases and eventually, diabetes related deaths.

References
International Diabetes Federation,(2019). IDF Diabetes Atlas (9thed.) International Diabetes Federation Joshi SR, S.B., & investigators.,S (2012). Prevalence of diagnosed and hypertension in India-results from screening India’s Twin Epidemic (SITE) study. PubMed.
About the author
|
Vivek Padgaonkar, former director,Project & Policy, OPPI, now independent Healthcare Consultant, working as an advisor to few Indian and MNCs in pharma & medical devices sector.
Prior to this, he had a long tenure at GSK almost over two decades in Sales & Marketing.
|
LSW LifeScienceWorld